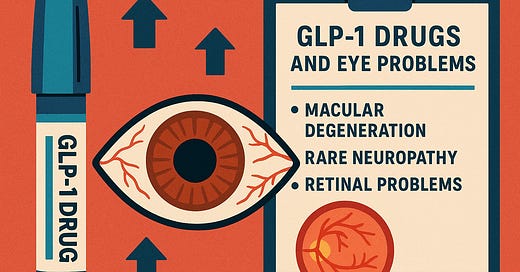
Focus on GLP-1 drugs & eye problems
I’m following a number of problems associated with GLP-1 drugs for overweight, obesity or Type 2 diabetes. By no means are my updates complete or conclusive. But they are collections of things I’ve read that many readers may not have heard anything about - perhaps because the overall weight of media messages on these drugs is on potential benefits. Yesterday, the respected STAT News’ Morning Rounds newsletter even asked, “What can’t GLP-1 drugs do?”
They’ve been shown to do a lot of good. But with that comes potential harms worth mentioning.
Today I offer a brief glimpse of seven reports in the past six months on eye problems associated with - but not proven to be caused by - the use of GLP-1 drugs.
Most of the following reports caught my eye on Medscape.com, which has done a good job tracking developments with this class of drugs. If you’re not seeing this kind of news coverage in your regular news sources, you may want to give Medscape a look.
In January, a paper in JAMA Ophthalmology reported nine cases of people who experienced eye problems while taking GLP-1 drugs - six on semaglutide and three on tirzepatide.
Seven had a form of neuropathy - nonarteritic anterior ischemic optic neuropathy or NAION. Some had progressive loss of vision.
One had diabetic papillitis (optic nerve swelling), did not lose vision and continued on the drug.
One had a condition that can affect blood flow to the retina.
The researchers wrote that although a causal link between the drugs and these problems cannot be established, they hypothesize that rapid lowering of high blood glucose may be at the root of the eye problems.
The American Academy of Ophthalmology has not recommended that patients stop using semaglutide, but rather, that patients experiencing vision loss while taking semaglutide should stop the drug and contact the physician prescribing the medication. The Academy has also suggested that a postmarketing surveillance study might better inform physicians and patients about the safety of semaglutide.
In March, another paper in JAMA Ophthalmology looked at optic nerve problems (NAION) among patients with Type 2 diabetes who took GLP-1 drugs. This was an analysis of about 175,000 records of people with diabetes who used semaglutide - compared with an equal number of people with diabetes who were taking other drugs unlike GLP-1 drugs. They found that the use of semaglutide was associated with a much greater risk of optic nerve problems than occurred in people taking other drugs. The authors emphasized the limitations of their findings, again with no proof that the drugs caused the problems.
In April, a paper in BMC Ophthalmology identified patterns of eye problems among people who took oral or injectable semaglutide. Researchers pulled data on 1,733 reports of eye problems associated with GLP-1 drug use from an FDA adverse event database. Problems occurred more often in women, and more often in people ages 45-64. Blurred vision and visual impairment were relatively high with both oral and injectable drugs. But retinal problems were more commonly associated with the injectable drugs. More than half of all adverse drug events were classified as not serious.
In June, a paper in JAMA Ophthalmology looked at age-related macular degeneration in people with Type 2 diabetes who were taking GLP-1 drugs. Researchers looked at data from 46,000 patients who had received a GLP-1 drug for at least six months, compared with 92,000 patients who had not taken these drugs. The data showed two times more cases of macular degeneration in the GLP-1 patients. There were 93 events in the smaller GLP-1 group, compared with 88 events in the twice-as-big non-GLP-1 group, yielding a 0.2% vs. 0.1% difference.
The authors concluded: “Further research is needed to determine if there is a true cause and effect relationship in the association identified in this investigation and to understand the trade-offs between the benefits and risks of GLP-1 RAs.”
Also in June, the European Medicines Agency safety committee warned that semaglutide (active substance in Ozempic, Rybelsus and Wegovy) may cause the NAION optic neuropathy described earlier in this article. The EU agency estimated that this condition may affect 1 in 10,000 people taking semaglutides for at least one year.
The agency has asked Novo Nordisk to list NAION as a side effect with a frequency of “very rare” in the product information that comes with the drugs. They say that:
If patients experience a sudden loss of vision or rapidly worsening eyesight during treatment with semaglutide, they should contact their doctor without delay. If NAION is confirmed, treatment with semaglutide should be stopped.
Some observers have opined that the European agency is stricter than the US Food and Drug Administration, which has not yet addressed this issue.
It’s important to note that just four days ago, a paper in the American Journal of Ophthalmology found that there was no significant increase in risk of NAION or (ischemic optic neuropathy) in patients taking semaglutide or GLP-1 drugs compared to control group patients with Type 2 diabetes or high BMI . Are your eyes glazed over yet?
This was the title of an editorial that accompanied the June paper in JAMA Ophthalmology described above:
The editorial writer concluded:
“GLP-1 RAs have had a tremendous role in the care of patients with diabetes and now those needing additional help with weight management. However, the adage that “there is no such thing as a free lunch” remains true. While certainly not outweighing the good these medications offer, prescribing physicians need to keep in mind the real and serious ocular adverse events that may occur.”
I hope this roundup provided you with some information that you didn’t previously have. The problems reported above are believed to be rare. It has not been proven that these drugs cause these problems. But what I accumulated here were reports that were all published in the last six months. So it certainly seems like an issue worth following.